description
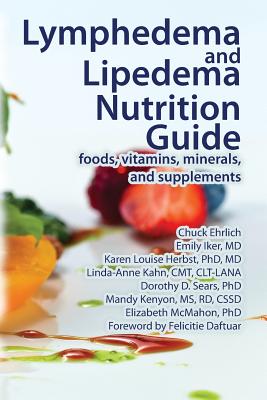
5Eat to starve lymphedema and lipedema by having foods that fight these conditions (and cancer) and avoiding foods that contribute to symptoms or related conditions. Learn how food choices affect both conditions and how better nutrition can improve symptoms (including pain) and delay changes associated with progression to more advanced stages. Intended for anyone with, or at risk for, lymphedema or lipedema, caregivers, lymphedema therapists, and other health care providers. Signs of lymphedema and lipedema (painful fat syndrome) include swelling (edema), abnormal fat accumulation, pain, skin changes, and infections (cellulitis, wounds or ulcers) in affected areas. Lymphedema and lipedema are progressive conditions that can be depressing, disfiguring, disabling, and (potentially) deadly, without treatment. This guide explains why nutrition is an essential part of treatment and self-care for these conditions, what to eat, and how to change your eating pattern. It also covers vitamins, minerals, and supplements that may be beneficial. You may be at risk for lymphedema if you have chronic venous insufficiency, other venous disorders, heart disease, obesity, a cancer diagnosis (especially breast cancer, reproductive system cancers, or melanoma), or a family history of lymphedema or swollen legs. Eating wisely and maintaining a healthy body weight can help reduce your risk of developing lymphedema symptoms. This guide includes all the information you need for changing your eating pattern including ways to increase your motivation and build support for changing your eating pattern, meal plans and recipes for recommended foods, a shopping guide, cooking tips, suggestions for eating away from home, and much more. It also includes detailed information on lymphedema and lipedema including risk factors, signs and symptoms, treatment, other health care considerations and more than 40 photos showing different stages of each condition. The authors include experts in lymphedema and lipedema treatment, nutrition research, and behavior change. Recommendations are based on the latest medical research combined with the clinical experience of the authors. In addition to sharing their clinical experience, Emily Iker and Linda-Anne Kahn share their personal insights from living well with lymphedema and lipedema, respectively. Chuck Ehrlich is a medical researcher and writer for LymphNotes.com, as well as a lymphedema caregiver. Emily Iker, MD, specializes in treating lymphedema and lipedema at the Lymphedema Center in Santa Monica and has lower-extremity lymphedema. Karen Louise Herbst, PhD, MD, treats people with lymphatic issues including lymphedema and lipedema, and leads the Treatment, Research and Education of Adipose Tissue (TREAT) Program, at the University of Arizona College of Medicine. Linda-Anne Kahn. CMT, NCTMB, CLT-LANA, CCN, is a lymphedema therapist, nutritional consultant and integrative health coach at Beauty Kliniek Day Spa and Wellness Center in San Diego, and has lipedema. Dorothy D. Sears, PhD, researches diet and behavior patterns for reducing disease risk at the University of California San Diego School of Medicine. Mandy Kenyon, MS, RD, CSSD, is a consulting dietitian and research leader for Salk Institute and Veteran's Medical Research Foundation. Elizabeth McMahon, PhD, is a clinical psychologist specializing in health-related behavior change and the author of several lymphedema books including Overcoming the Emotional Challenges of Lymphedema. Foreword by Felicitie Daftuar, founder and executive director of Lipedema Foundation and past-president of the Fat Disorders Research Society (FDRS.org).
member goods
No member items were found under this heading.
listens & views
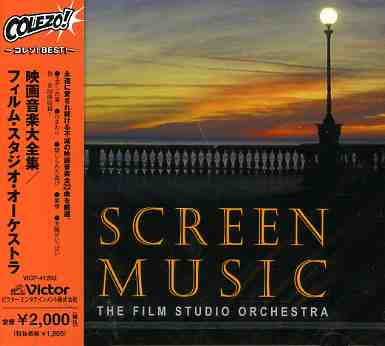
COLEZO! CINEMA MUSIC / O.S.T. ...
by COLEZO! CINEMA MUSIC / O.S.T. (JPN)
COMPACT DISCout of stock
$19.99
Return Policy
All sales are final
Shipping
No special shipping considerations available.
Shipping fees determined at checkout.